Plantar Heel Pain (Plantar Fasciitis) Best Practice Guidelines
Following the publication of the paper “Management of plantar heel pain: a best practice guide informed by a systematic review, expert clinical reasoning and patient values” by Morrissey et al, our blog will highlight the key takeaways and how this can influence your clinical practice.
Who Is Most Likely To Get Planter Heel?
Plantar heel pain (PHP) is most commonly found in inactive middle to older aged people. Heel pain can exist as pain that starts after rest and increases or decreases with activity. Working out which type of heel pain your patient has relies on a solid history and physical exam.
Key points to consider about Planter Heel Pain:
- Increase in activity level
- Increase in weight
- Acute incident/injury
- Other causes (inflammatory, tendinopathy, neuropathic)
- Insidious onset
- Conditions That Cause Plantar Heel Pain
Conditions that cause PHP such as plantarfasciopathy, heel bursitis (subcalcaneal bursitis), heel bumps, tarsal tunnel syndrome, chronic inflammation of the heel pad, calcaneal fracture, Sever’s disease (calcaneal apophysitis), Achilles tendinosis should all be considered during assessment.
There are a lot of studies looking at various treatment modalities but this is the first to review them all and combine them with expert opinion and patient input.
(Just as a refresher… *itis – inflammation *osis – degenerative change *opathy – change in)
The authors set out the criteria for selecting studies that included type of study, characteristics of participants, types of interventions and outcome measures. From the data collection and analysis that followed 362 studies were assessed and 51 studies met the criteria to be included.
Next the authors arranged semi-structured interviews with 14 expert clinicians from around the world. These clinicians were on average treating 9 PHP patients per month and had an average of 51 publications each.
The authors surveyed patients using an online questionnaire to explore their experiences of treatment related to PHP.
Best Approach to Plantar Heel Pain
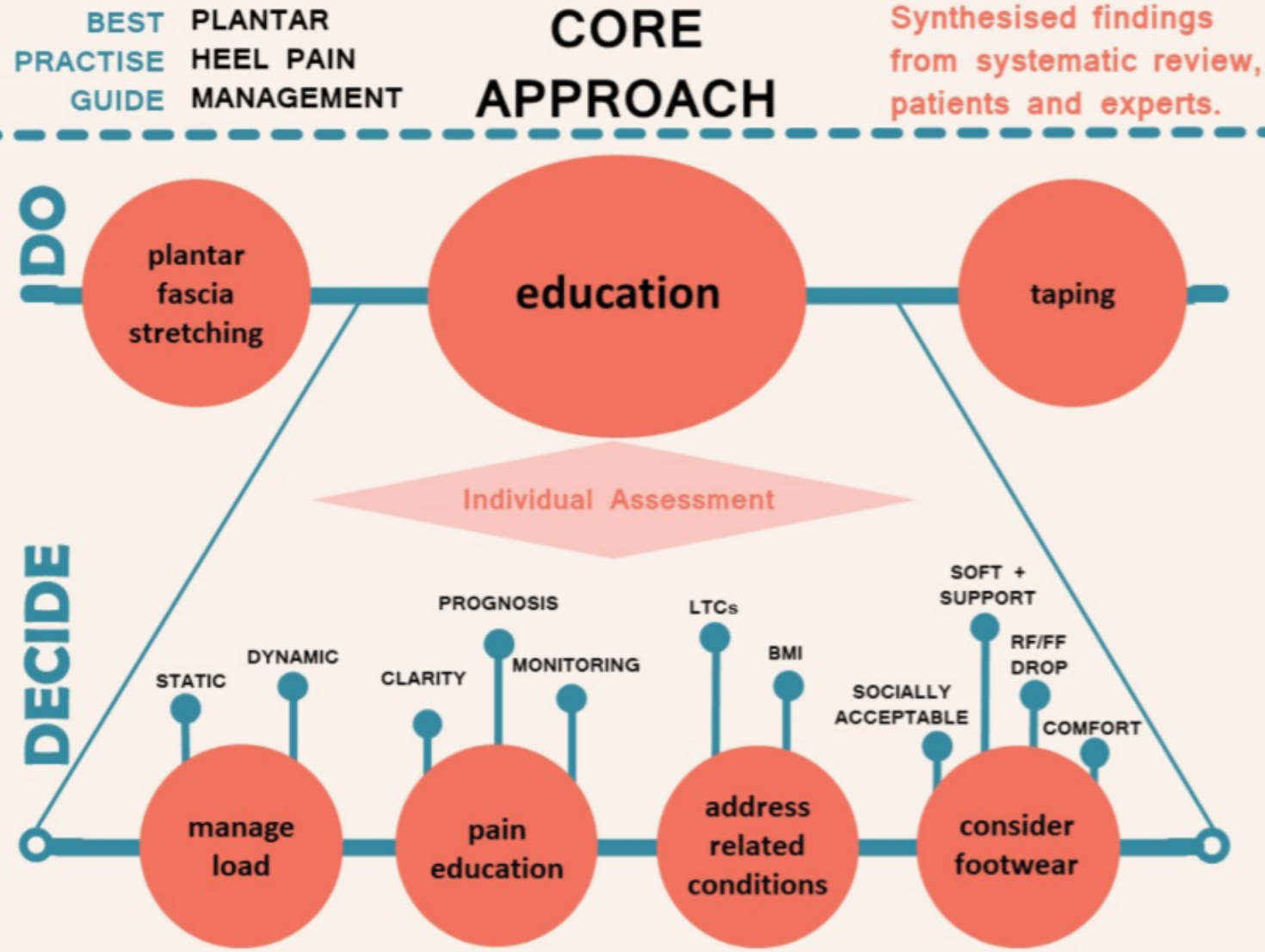
From the data collected in the 3 categories the authors came up with the “Core Approach”. They recommended that all first line intervention (DO) includes plantarfascia taping and stretching as these areas provided strong evidence of effectiveness. Furthermore, the authors advise patient education (DECIDE).
It’s highlighted as a key factor for a positive outcome. The 4 categories for patient education of load management, pain education, related conditions and footwear should be discussed dependent on the patient assessment.
How Effective Is The Core Approach To Resolving Plantar Heel Pain?
As an example, load management to reduce the amount of running a person is doing per week to enable the plantarfascia stretching and taping to be effective or reducing the amount of standing someone may be doing on a daily basis. These may then be combined with footwear advice and/or pain education.
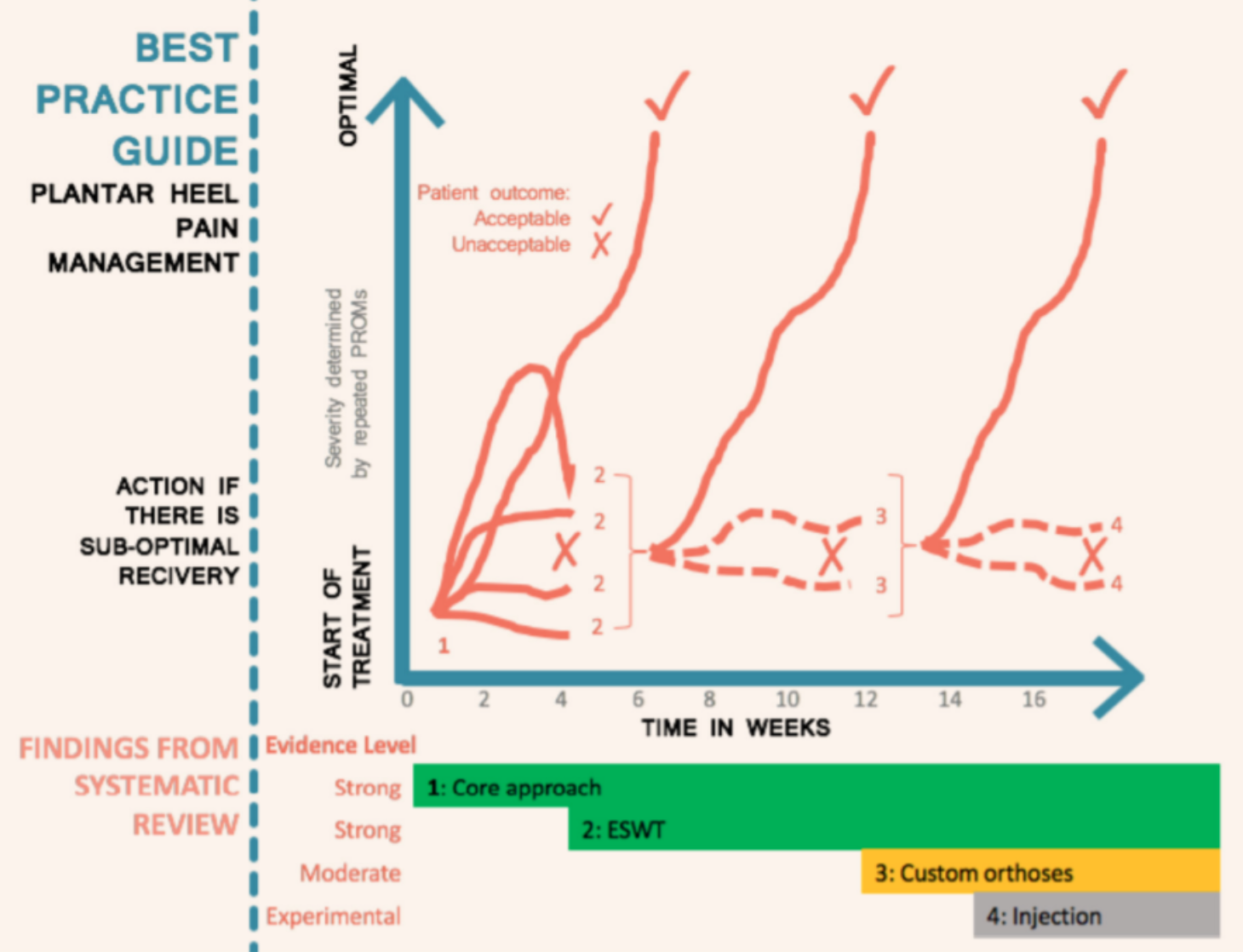
According to the Core approach, following a 4 to 6 week period if symptoms are not responding to these treatments it’s recommended progressing to Extracorporeal Shockwave Therapy (ESWT). ESWT has strong evidence of effectiveness for symptoms that are persisting. Foot orthoses are then recommended later (approximately week 12) and can be used alongside the Core approach and ESWT if symptoms continue.
However, there are no reported specifics for prefabricated or custom and no reference to material choices for either type of orthoses.
Its recommended orthoses are prescribed based on assessment of the patient.
Dry needling is not recommended as a first line intervention and also has a neutral evidence level. Corticosteroid and platelet rich plasma injection therapy are commonly used but have a low evidence level. Resistance exercise has no evidence in relation to PHP, however has been seen to be effective in hip and knee osteoarthritis and other tendonopathies.
To summarise the guidelines:
- Core approach (first line)
- DO prescribe plantarfascia stretching and taping
- DO educate patients on the relevant areas related to their symptoms
- Progress to ESWT for persistent symptoms
- Consider foot orthoses after ESWT
- Consider experimental options further down the line if symptoms continue for more than 12 weeks